Clinico-pathological Characteristics of Cutaneous Malignant Melanoma in Pakistan
By Romaisa Shamim Khan1, Osama Shakeel2, Ahmad Faraz Bhatti1, Raza Hussain3Affiliations
doi: 10.29271/jcpsp.2020.11.1197ABSTRACT
Objective: To analyse epidemiological and clinical characteristics of patients presenting with cutaneous malignant melanoma (CMM) in Pakistan; and to compare the results with other studies.
Study Design: Case series.
Place and Duration of Study: Shaukat Khaum Memorial Cancer Hospital (SKMCH) from January 1997 to December 2017.
Methodology: All patients presenting to the study centre with a diagnosis of CMM were included in the study. Non-cutaneous melanoma cases were excluded. Patient demographics, tumor type, and tumor stage were recorded retrospectively. All data were analysed in SPSS and descriptive statistics were determined.
Results: A total of 169 CMM patients were registered during a 20-year period. The highest incidence of melanoma was seen in the age group 40-59 years (n=69, 40.8%). Most common clinical subtype was unspecified melanoma (n=154, 91%). The most frequently observed T-stage at presentation was Tx (n=124, 73.4%), followed by T4 (n=23, 13.6%). With regard to body distribution, CM was seen most commonly in the lower limb including hip.
Conclusion: CMM is a rare disease in Pakistan. However, patients tend to present at a more advanced stage. Identification of risk factors and tumor characteristics is, therefore, of paramount importance in managing these patients.
Key Words: Cutaneous malignant melanoma (CMM), Pakistan, Lower middle income country, Stage.
INTRODUCTION
Malignant melanoma is a cancer, arising from the pigment-producing cells (melanocytes) in the skin. Though it accounts for less than 5% of all cutaneous malignancies, it has the highest mortality rate of all skin cancers.1 It is responsible for upto 80% of deaths caused by cutaneous malignancies.2
According to estimates for 2008, there were almost 200,000 new cases of invasive CMM globally, and an estimated 46,000 deaths from the disease.3 The vast majority of cases (almost 85%) occur in developed countries, where melanoma ranks overall as the sixth most frequently diagnosed cancer.4 Fair-skinned populations of the Scandinavian countries have some of the highest rates of CM incidence in the world.5
A significant increase in the incidence of CM has been observed globally in the past few decades,6 despite educational programmes aimed at prevention strategies. This increase can be attributed to a general change in attitude, from sun-avoidance toward sun-seeking behaviour.7 Considering the high morbidity and mortality associated with the disease, this is undoubtedly a cause of concern.8
The etiology of CM is an interplay between environmental, genetic and individual host factors, as evidenced by findings from seminal migrant studies.9 Risk factors associated with its development include fair skin and hair, light eyes, Caucasian lineage, large numbers of acquired nevi, presence of atypical nevi, personal or family history of CM, advanced age, male gender, xeroderma pigmentosum, sunburn, and increased exposure to ultraviolet radiation.10,11
Recognition of general and specific risk factors in various demographical locations is crucial from both the clinical and public health perspective. Unfortunately, there are limited studies available to provide knowledge regarding incidence and other characteristics of melanoma from Pakistan.12,13 This is due to unreliable centralised cancer-registries, deficiency of compulsory notification, and lack of health-seeking behaviour in the general public, especially the elderly population.14 To reduce the morbidity and mortality associated with CMM in Pakistan, there is a need to identify risk factors unique to this population.
The objective of this study was to analyse the clinical characteristics of patients presenting with CMM at a dedicated cancer hospital in Pakistan.
METHODOLOGY
This was a case series done at Shaukat Khaum Memorial Cancer Hospital (SKMCH), a dedicated cancer hospital. Database search was performed to identify all patients registered at SKMCH with the diagnosis of melanoma, over a 20-year period, from January 1997 to Dec 2017. Patients who had cutaneous malignant melanoma, or cutaneous melanoma (CM) were filtered from these cases and studied. All non-cutaneous melanomas were excluded. Detailed review of the charts was performed for all the CM patients. Patients’ demographics were recorded, including age, gender and area of residence. Individuals were grouped into 5 age-classes: ≤19, 20-39, 40-59, 60-79, ≥ 80. The following tumor characteristics were studied: Area localisation in the body, T-stage at presentation, and tumor histology. The retrieved data were entered in the Excel spreadsheet and then exported to the SPSS version.20.0 for statistical analysis. Quantitative variables were expressed as mean. Categorical variables were described by frequencies and percentages.
Table I: Demographics of patients with cutaneous melanoma.
|
|
Men |
Women |
Total |
|
Total No. (%) |
98 (58%) |
71 (42%) |
169 (100%) |
|
Mean age in years (SD) |
47.6 (17.0) |
47.4 (16.7) |
47.5 (16.8) |
|
Age groups: ≤19 years 20 – 39 years 40 – 59 years 60 – 79 years ≥ 80 years |
4 (4.1%) 27 (27.6%) 40 (40.8%) 24 (24.5%) 3 (3.1%) |
3 (4.2%) 21 (29.6%) 29 (40.8%) 15 (21.1%) 3 (4.2%) |
7 (4.1%) 48 (28.4%) 69 (40.8%) 39 (23.1%) 6 (3.6%) |
|
Resident of: KPK Punjab Sindh Baluchistan Azad Kashmir Afghanistan |
30 (30.6%) 61 (62.2%) 3 (3.1%) 3 (3.1%) 0 (0.0%) 1 (1.0%) |
15 (21.1%) 49 (69.0%) 1 (1.4%) 1 (1.4%) 1 (1.4%) 4 (5.6%) |
45 (26.6%) 110 (65.1%) 4 (2.4%) 4 (2.4%) 1 (0.6%) 5 (3.0%) |
RESULTS
A total of 169 patients with CM were admitted in 20 years. There were 98 males (58%) and 71 females (42%). The mean age of the study population was 47.5 years (5-91 years). The most common age-group affected, for both genders, was 40-59 years. Majority of the patients belonged to the northern half of the country, with the highest number hailing from the province of Punjab (Table I).
Lower limb was found to be the most common body region affected by CM (n=83, 49.1%), followed by the head and neck region (n=43, 25.4%). Regarding T-stage, Tx was the predominant finding. Amongst those in which the T-stage was documented, T4 was found to be the most common stage at presentation. Most common histologic type was unspecified, followed by the nodular type (Table II).
In this study, the yearly incidence of CM has been 6 cases (4-23) per year between 1997 and 2017 (Figure 1). The surge seen in 2017 coincided with the establishment of a regular cutaneous malignancy service in the hospital.
Table II: Tumor characteristics.
|
Tumor characteristics |
Men |
Women |
Total |
|
Body site: Head and neck Arm and shoulder Leg and hip Trunk |
33 (33.7%) 6 (6.1%) 47 (48.0 %) 12 (12.2%) |
10 (14.1%) 9 (12.7%) 36 (50.7 %) 16 (22.5%) |
43 (25.4%) 15 (8.9%) 83 (49.1%) 28 (16.6%) |
|
T stage at presentation: T1 T2 T3 T4 Tx |
1 (1.0%) 6 (6.1%) 6 (6.1 %) 16 (16.3%) 69 (70.4%) |
1 (1.4%) 3 (4.2%) 5 (7.0 %) 7 (9.9%) 55 (77.5%) |
2 (1.2%) 9 (5.3%) 11 (6.5 %) 23 (13.6%) 124 (73.4%) |
|
Tumor histology: Melanoma, unspecified Nodular Superficial spreading Amelanotic |
88 (89.8%) 9 (9.2%) 1 (1.0 %) 0 (0.0%) |
66 (93.0%) 3 (4.2%) 1 (1.4 %) 1 (1.4%) |
154 (91.1%) 12 (7.1%) 2 (1.2 %) 1 (0.6%) |
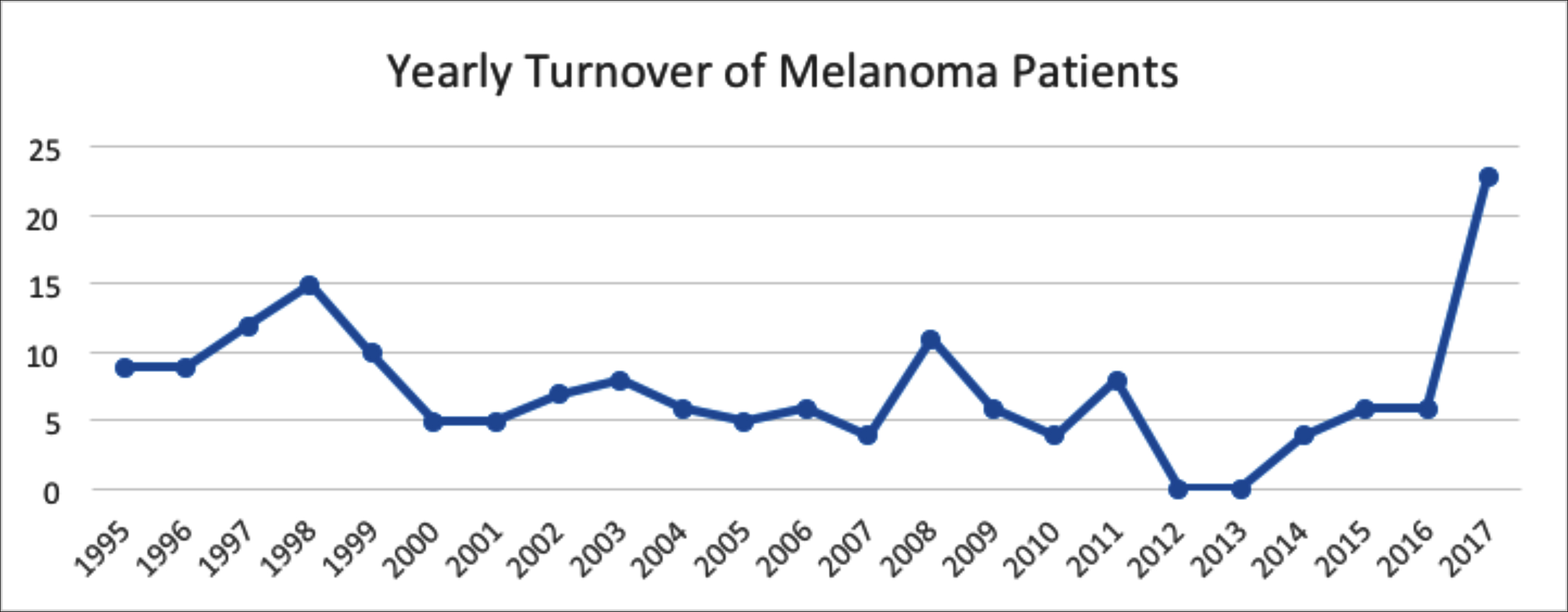 Figure 1: Illustrating the yearly turnover of melanoma patients at SKMCH & RC.
Figure 1: Illustrating the yearly turnover of melanoma patients at SKMCH & RC.
DISCUSSION
This study indicated that CMM is not so rare in this part of the world. CM is more common in fair-skinned Caucasian populations, with the highest incident rates seen in Australia15 and Nordic countries.5 Unfortunately, due to lack of centralised reporting, it is not possible to ascertain the true incidence of CM in Pakistan.
CMM can be a big burden on healthcare in lower-middle income countries like Pakistan. The reason for that is three-fold. Firstly, people of the northern areas of Pakistan have fairer skin and light-colored eyes, falling into globally established high-risk categories.However, it also affects darker skinned individuals from Punjab and Sindh. Secondly, lack of awareness and inconsistencies in primary healthcare system means that patients present at more advanced stages than their western counterparts. Thirdly, there is evidence to suggest that when melanoma occurs in darker-skinned individuals, it behaves more aggressively, and their survival time would be significantly lower than that in Caucasians.16
As such, there are no existing data that describe clinico-pathological features of CM in Pakistan, nor are there any studies that identify potential risk factors specific to our population. This is the first study to report a comprehensive view of clinico-pathological characteristics of CM in Pakistan.
Median number of patients presenting was 8 per annum during this period, with a definite surge seen in the year 2017. This can be attributed to the fact that a full time plastic surgery service at SKMCH began in 2017 and a dedicated cutaneous MDT Board and (multi-disciplinary tumor board) was started. However, it is pertinent to mention here that it is a specialised cancer hospital and receives referral from all over the country as well as adjacent countries. Therefore, it is not possible to infer incidence and prevalence of melanoma in our community, based on this data. It does, however, serve as a useful source to study the pathological characteristics and clinical profiles of patients presenting with melanoma.
In this study, the mean age at diagnosis of CM was 47.5 years. This is lower than the mean ages reported in other studies.17,18 A higher incidence of melanoma was observed in male patients. Several authors have suggested that melanoma affects men and women differently. In the western population, young and adolescent females are more susceptible to melanoma than their male counterparts.19 This may be due to the use of indoor tanning among females. This is not a common practice in Pakistan. After the age of 40, incidence in males is reported to be higher than in females. The same was observed in this study.18,20,21
The relationship of anatomic location (and thus sun exposure), to development of melanoma is more complex than it seems. Green proposed the theory of site-dependent susceptibility of melanocytes to malignant transformation.22 According to him, essentially there are two types of people. Those with a low propensity for melanocyte proliferation will develop melanomas in chronically sun-exposed areas. Conversely, people with a high propensity for melanocyte proliferation (as evidenced by high numbers of nevi) will develop melanoma in areas which are intermittently exposed to the sun, such as the trunk. In our study, the lower limbs were most commonly affected in both genders, followed by the head and neck region. Both these areas will constitute chronically sun-exposed skin.
T-stage at presentation was determined with the Breslow thickness that was documented on the initial biopsy. Unfortunately, it was only documented in 36% of the biopsy reports. Out of these documented cases, T4 was the most prevalent stage at presentation. This emphasises a common problem that is faced in all aspects of healthcare in the developing world: Late presentation and failure of implementation of screening modalities. Moreover, majority of the biopsy reports did not mention the tumor histological type. This, as well as the lack of mentioning the Breslow thickness was more so in the earlier years, and an improvement in documentation of these findings was seen in the more recent biopsies.
Most of the patients belonged to the northern half of the country, with the maximum number presenting from Punjab and KPK. We feel that it is due purely to logistic reasons, such as ease of access to the hospital, and therefore any conclusions regarding geographical variations cannot be drawn from this information.
CONCLUSION
CM though considered a disease of the fair-skinned, is fairly common in Pakistan. It tends to be more aggressive in behaviour in darker-skinned populations. This, along with the fact that our patients present late, makes it a significant healthcare burden. Identification of common risk factors, and an understanding of tumor characteristic specific to our population, is essential for implementing preventive and screening programmes at the national level.
ETHICAL APPROVAL:
Approval was obtained from the Institutional Review Board of Shaukat Khanum Memorial Cancer Hospital and Research Centre.
PATIENTS' CONSENT:
Waiver of the consent was obtained from the Institutional Review Board of Shaukat Khanum Memorial Cancer Hospital and Research Centre.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS' CONTRIBUTION:
RSK: Study design and manuscript writing,
OS: Concept of study, data collection, data analyses and manuscript writing.
AFB, RH: Study lead and supervision.
All authors have approved the final manuscript
REFERENCES
- Cancer Research UK. Skin cancer incidence statistics. London: Cancer Research UK: May 2014. http:/www.cancer researchuk.org/cancerinfo/cancerstats/types/skin/incidence
- Azarjana K, Ozola A, Ruklisa D, Cema I, Rivosh A, Azaryan A, et al. Melanoma epidemiology, prognosis and trends in Latvia. J Eur Acad Dermatol Venereol 2013; 27(11):1352-9. doi: 10.1111/jdv.12007.
- Ferlay J, Shin H, Bray F. Globocan 2008 v1.2, cancer incidence and mortality worldwide: IARC cancerbase No. 10. Lyon, France: International Agency for Research on Cancer, 2010.
- Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin 2006; 56(2): 106-30. doi.org/10.3322/canjclin.56.2.106.
- Eco.iarc.fr [Internet] Malignant melanoma of skin. Lyon: International Agency for Research on Cancer EUCAN; [2015 nov 15]. Available from: http://eco.iarc.fr/eucan/Cancer. aspx? Cancer=20#blockmapa.
- Van der Leest RJ, Flohil SC, Arends LR, de Vries E, Nijsten T. Risk of subsequent cutaneous malignancy in patients with prior melanoma: A systematic review and meta-analysis. J Eur Acad Dermatol Venereol 2015; 29(6):1053-62. doi: 10.1111/jdv.12887.
- Richardson A, Fletcher L, Sneyd MJ. The incidence and thickness of cutaneous malignant melanoma in New Zealand 1994–2004. N Z Med J 2008; 121(1279):18-26.
- Rampen FH, Neumann HA, Kiemeney LA. Fundamentals of skin cancer/melanoma screening campaigns. Clin Exp Dermatol 1992; 17(5):307-12. doi:10.1111/j.1365- 2230.1992.tb00217.x.
- Graham B, Asbjorn A. Incidence of malignant melanoma of the skin in Norway, 1955–1989: Association with solar ultraviolet radiation, income and holidays abroad. Int J Epidemiol 1996; 25(6):1132–8. doi: 10.1093/ije/25.6.1132.
- Vries E, Bray F, Coebergh JW. Melanocytic tumours. In: LeBoit PE, Burg G, Weedon D, Sarasin A, editors. World Health Organization classification of tumours: Pathology and genetics, skin tumour. 3rd ed. Lyon: International Agency for Research on Cancer; 2006. pp. 49–120.
- Kocarnik JM, Park SL, Han J, Dumitrescu L, Cheng I, Wilkens LR, et al. Replication of associations between GWAS SNPs and melanoma risk in the population architecture using genomics and epidemiology (PAGE) study. J Invest Dermatol 2014; 134(7):2049-52. doi: 10.1038/jid.2014.53.
- Ahmed A, Alam MB, Khan W, Badar A, Shah SH. Frequency and characteristics of skin cancers diagnosed at Ayub Medical College, Abbottabad, Pakistan from 1995-2003. J Ayub Med Coll Abbottabad 2007; 19(4):3-6.
- Sarfraz T, Tariq H, Iftikhar N, Raza N, Malik NA, Khan SA, et al. Frequency and histological pattern of malignant skin lesions in Pakistani population. Pakistan Armed Forces Med J 2019; 69(1):83-6.
- Ladha A, Khan RS, Malik AA, Khan SF, Khan B, Khan IN, et al. The health seeking behaviour of elderly population in a poor-urban community of Karachi, Pakistan. J Pak Med Assoc 2009; 59(2):89-92.
- Canceraustralia.gov.au [Internet] Melanoma of the skin statistics. Surry Hills: Australian Government, Cancer Australia; [2015 Nov 15]. Available from: http://www. uptodate.com/contents/onychomycosis?source=search_result&search=onicomicose&selectedTitle=1%7E23 statistics.
- Shoo BA, Kashani-Sabet M. Melanoma arising in African, Asian, Latino- and Native-American populations. Semin Cutan Med Sur 2009; 28(2):96-102. doi: 10.1016/j.sder. 2009.04.005.
- A new understanding in the epidemiology of melanoma Esther Erdei and Salina M Torres. Expert Rev Anticancer Ther 2010; 10(11):1811-23. doi: 10.1586/era.10.170
- Surveillance, epidemiology, and end results (SEER). Program cancer statistics review, 1975–2013, National Cancer Institute [Internet] Nov, 2015. SEER data submission [cited posted to the SEER web site, 2016 Apr]. Available from:http://seer.cancer.gov/csr/1975_2013/
- Weir HK, Marrett LD, Cokkinides V, Barnholtz-Sloan J, Patel P, Tai E, et al. Melanoma in adolescents and young adults (ages 15–39 years): United States, 1999–2006. J Am Acad Dermatol 2011; 65(5) Suppl 1:S38-49. doi: 10.1016/ j.jaad.2011.04.038.
- Watson M, Geller AC, Tucker MA, Guy GP Jr. Weinstock MA. Melanoma burden and recent trends among non-Hispanic whites aged 15–49 years, United States. Prev Med 2016; 91:294-8. doi: 10.1016/j.ypmed.2016.08.032.
- Garbe C, Leiter U. Melanoma epidemiology and trends. Clin Dermatol 2009; 27(1):3-9. /doi.org/10.1016/ j.clindermatol. 2008.09.001.
- Green A. A theory of the site distribution of melanomas: Queensland, Australia. Cancer Causes Control. 1992;3(6): 513–6.